10 common baby + child illnesses and remedies

We rounded up the top 10 illnesses that babies and kids get (including our own!) and some descriptions to help you understand what they are and when to seek treatment. Please remember, this is meant for educational purposes and is not meant to take the position of your provider. Keep reading to learn more!
Disclaimer: This is intended for educational and resource purposes only, not to diagnose or treat your child. Please call your child’s provider immediately if you are concerned or have questions related to your child’s health including illness and treatment.
1. Roseola
- What is it?
A virus commonly seen in children 6 months – 3 years old - Symptoms:
- High fever for 3-5 days (101-104 degrees F)
- After the fever breaks, a distinctive full body rash appears 12-24 hours later.
- Rash is flat and equal on sides of body, commonly seen on the chest, and stomach but can spread to arms and legs. The rash is not itchy and goes away in 2-3 days.
- Treatment:
- There is no treatment for the virus.
- Management of the fever is very important.
- Keep your child hydrated and you can use fever reducing medications (infant or children’s Motrin and/or Tylenol – see our sick baby and toddler recommendations here). Please contact your provider for accurate doses. Please note that children under 6 months of age cannot receive Motrin (ibuprofen).
- When to seek help:
- If rash becomes purple/blood colored with fever- call 911 (without fever go to ER)
- Call your pediatrician if the fever returns after the rash appears or rash lasts longer than 4 days
2. Hand Foot and Mouth Disease (HFMD)
- What is it?
A common, contagious virus commonly seen in children 6 months – 4 years old - Symptoms:
- Small red blisters and/or spots seen on the palms of hands and bottom of feet that last up to 10 days.
- Can present with painful ulcers in the mouth or on the tongue and groin and last up to 7 days.
- A common place for HFMD to start is the diaper area! See Kate’s Diaper Rash Remedy for cure.
- Often, it will be painful for babies to drink bottles/nurse
- A low grade fever can also be present for 2-3 days.
- If severe can spread to arms and legs.
- Finger and toenails sometimes will peel off after the infection is over.
- Treatment:
- There is no treatment for the virus.
- Management of the fever is very important.
- Keep your child hydrated and can use fever reducing medications (Motrin and/or Tylenol – see our sick baby and toddler product recommendations here). Please contact your provider for accurate doses. Please note that children under 6 months of age cannot receive Motrin (ibuprofen).
- Fluids and a soft diet for those who have mouth ulcers. These are painful so using pain relieving medication (Tylenol or Motrin) can help.
- Some tricks for older babies and toddlers to stay hydrated:
- Pedialyte popsicles
- Pedialyte slushie (blend with ice)
- Clear juice (apple or pear) slushie
- Breastmilk popsicles (try this popsicle mold)
- Antacid can be used to soothe mouth (1 years old +). Contact your provider before giving. A prescription medication called Magic Mouth Wash can also be used if sores are causing significant pain.
- The blisters do not need special treatment, however, if they do open, the fluid is contagious to others. You can cover with Aquaphor to help heal.
 **Please note that adults can get HFMD!
**Please note that adults can get HFMD!
- When to seek help:
- Stiff neck, weakness, severe headache, trouble walking are all signs to go to the ER.
- Call your pediatrician if the fever lasts more than 3 days, child shows signs of dehydration, is seemingly getting worse.
- Dehydration signs in babies and toddlers: dry mouth and tongue, no tears when crying, no wet diapers for three hours, sunken eyes or cheeks, listlessness or irritability. Click here to read more about signs of dehydration.
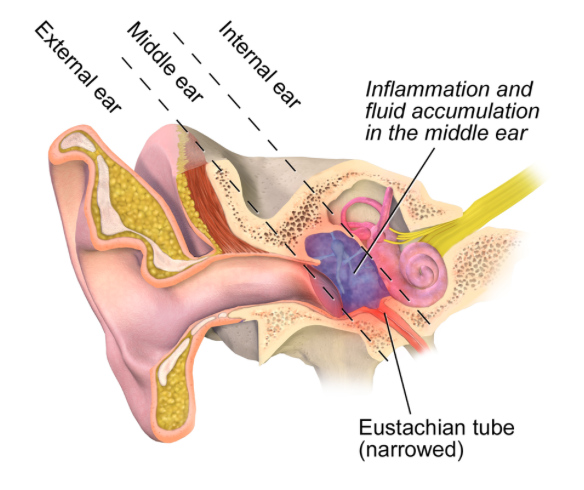
3. Ear Infection
- What is it?
- A very common infection in the middle ear (behind the eardrum) most commonly seen in children 6 months – 2 years old (however still seen in children up to age 8). Ear infections can be bacterial or viral.
- Usually associated with a cold and the ear infection will start around day 3 of the cold. This infection is NOT contagious.
- Symptoms:
- A very painful earache.
- In younger children fussiness, disturbance of sleep, tugging at ears.
- About half will get a high fever with the ear infection. Fever should only last about 2 days.
- Eye drainage can also be a sign of ear infections
- Treatment:
- If suspected to be bacterial, an antibiotic will be prescribed by your provider.
- The infection should start to be better in 2-3 days.
- Management of the fever and pain is used with Tylenol or Motrin. Please contact your provider for accurate doses. Please note that children under 6 months of age cannot receive Motrin (ibuprofen).
- You can also use a cold compress to relieve pain.
- Make sure your child stays hydrated
- Some tricks for older babies and toddlers to stay hydrated:
- Pedialyte popsicles
- Pedialyte slushie (blend with ice)
- Clear juice (apple or pear) slushie
- Breastmilk popsicles (try this popsicle mold)
- Some tricks for older babies and toddlers to stay hydrated:
- See our sick baby and toddler product recommendations here!
- When to seek help:
- If child becomes weak and cannot stand, go to ER.
- Call provider at the onset of the ear infection to get a prescription for antibiotics, extremely high fever, pain not relieved with medication, stiff neck, or if fever lasts more than 48 hours after starting antibiotic.
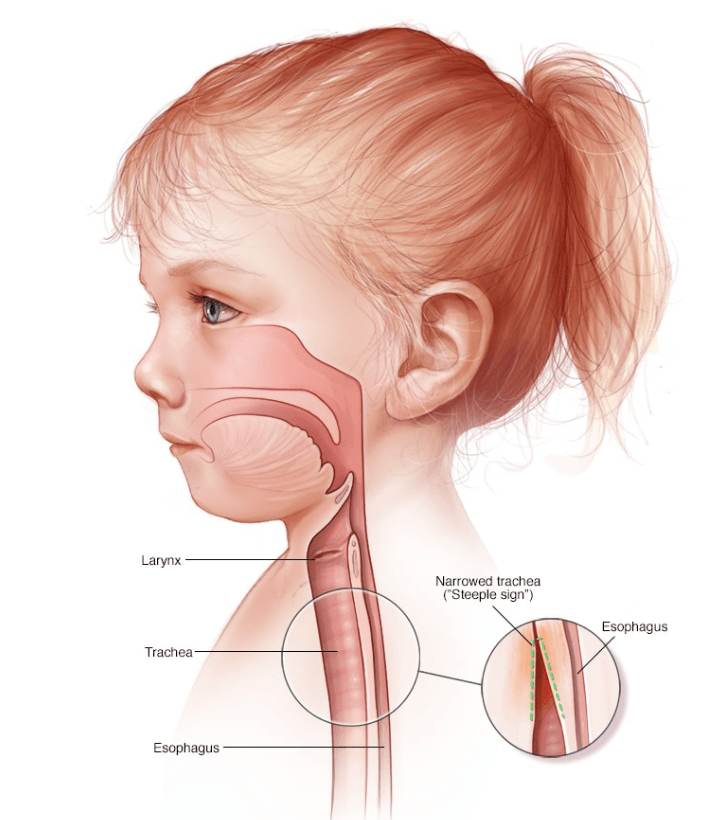
4. Croup
- What is it?
- There are several types of croup but the most common is caused by a virus that affects the larynx (voice box).
- Severe cases can cause swelling of the airway.
- Lasts up to 6 days with symptoms and is worse at night. The cough can last up to 2 weeks.
- Symptoms:
- Barky cough (sounds like a seal), fever, stridor (noisy high-pitched breathing- THIS IS SERIOUS AND YOU SHOULD CONTACT YOUR PROVIDER ASAP!)
- Treatment:
- Cool mist humidifier only – no heat! Heat can cause Fever reducing medications if above 102 degrees).
- Increase fluid intake.
- Some tricks for older babies and toddlers to stay hydrated:
- Pedialyte popsicles
- Pedialyte slushie (blend with ice)
- Clear juice (apple or pear) slushie
- Breastmilk popsicles (try this popsicle mold)
- If serious with noisy breathing, the provider may give an oral steroid to help with the swelling in the airway. See our sick baby and toddler product recommendations here.
- When to seek help:
- Severe trouble breathing, passing out, blue coloring to lips, drooling (not due to teething)- call 911.
- Call doctor if your child has trouble breathing but not severe, non-stop coughing, fever greater than 104 degrees, fast breathing, chest or neck pain, or you feel your child is very ill.
5. UTI (urinary tract infection)
- What is it?
- The most common UTI is a bacterial infection of the bladder.
- More common in girls than in boys due to a shorter urethra in girls.
- Usually due to stool coming in contact with the urethra.
- Usually starts to feel better after 48 hours of antibiotics.
- Symptoms:
- Burning, stinging pain with urination, urine frequency (small amount of urine very often).
- Urgency (trouble holding urine).
- fever, flank pain (side of body below the ribs) indicating a kidney infection.
- Foul smelling or bloody urine.
- Treatment:
- Antibiotic, pain and fever reducing medications
- Management of the fever and pain is used with Tylenol or Motrin. Please contact your provider for accurate doses. Please note that children under 6 months of age cannot receive Motrin (ibuprofen).
- You can also use a cold compress to relieve pain.
- Make sure your child stays hydrated
- Some tricks for older babies and toddlers to stay hydrated:
- Pedialyte popsicles
- Pedialyte slushie (blend with ice)
- Clear juice (apple or pear) slushie
- Breastmilk popsicles (try this popsicle mold)
- See our sick baby and toddler product recommendations here)
- Some tricks for older babies and toddlers to stay hydrated:
- Increase fluid intake, avoid soaps, bubble bath, or shampoo near vulva.
- When to seek help:
- If the child can’t stand or if you feel they have a life threatening emergency- call 911.
- If the child cannot pass urine – go to ER.
- Call doctor if fever, chills, flank pain, vomiting interfering with taking antibiotic, blood in urine, symptoms are getting worse.
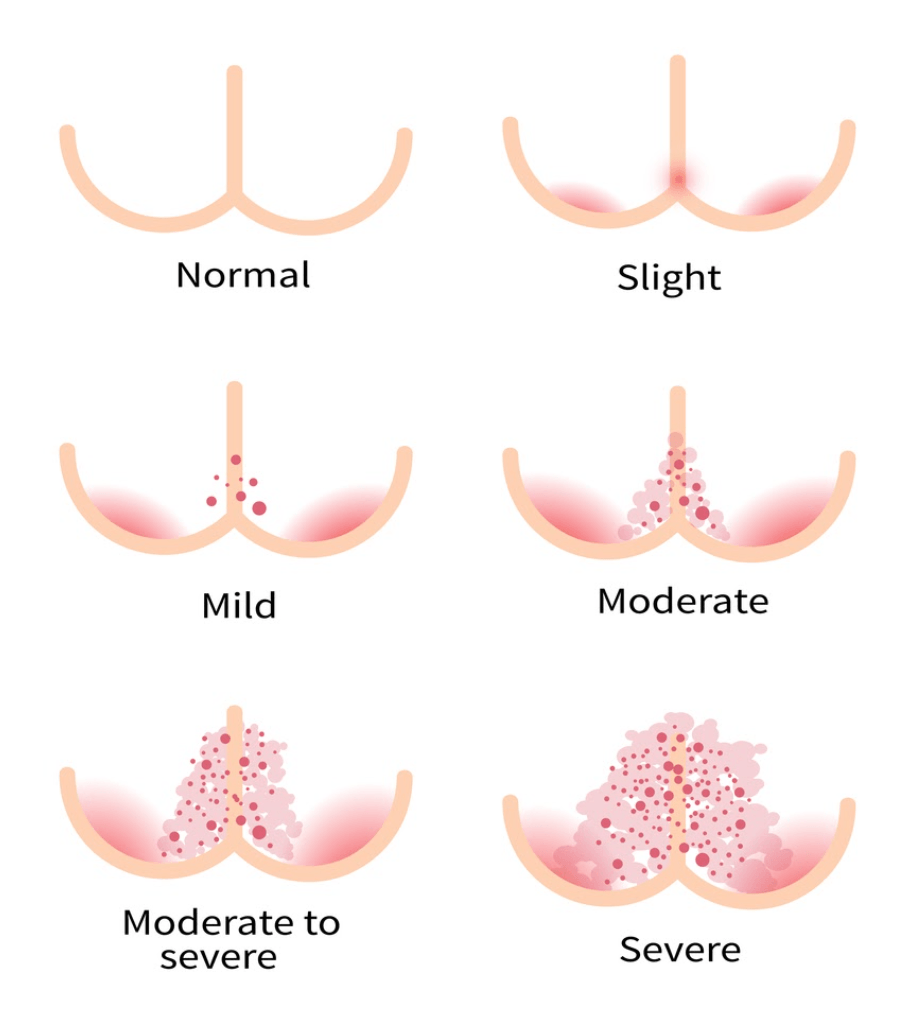
6. Diaper rash
- What is it?
- Any type of rash or skin irritation in the diaper-covering area.
- Most effects children age 0-3 years old or children still in diapers.
- Caused by POOP!
- Symptoms:
- Mild rashes usually appear as pink/reddened, dry skin in the diaper area.
- Severe rashes typically appear very red, raw, open skin and/or sores and sometimes bleeding.
- Babies with diaper rashes may be fussy and have disrupted sleep.
- Pain with urination.
- Treatment:
- Frequent diaper changes, remove stool (by GENTLY PATTING ((don’t rub!)) with room temperature water wipes or wash cloth) from all areas of skin including skin folds
- Expose baby’s bottom to air as much as possible
- Kate’s diaper rash remedy!, If rash is bright red and hasn’t improved within 3 days, call your doctor!
- When to seek help:
- Diaper rashes that are frequently recurring or won’t go away after greater than 3 days
- The rash could be fungal and you will need a Rx cream
- Diaper rash accompanied by a fever, bright red skin that peels off in sheets, open sores/blisters, your child is looking/acting very sick
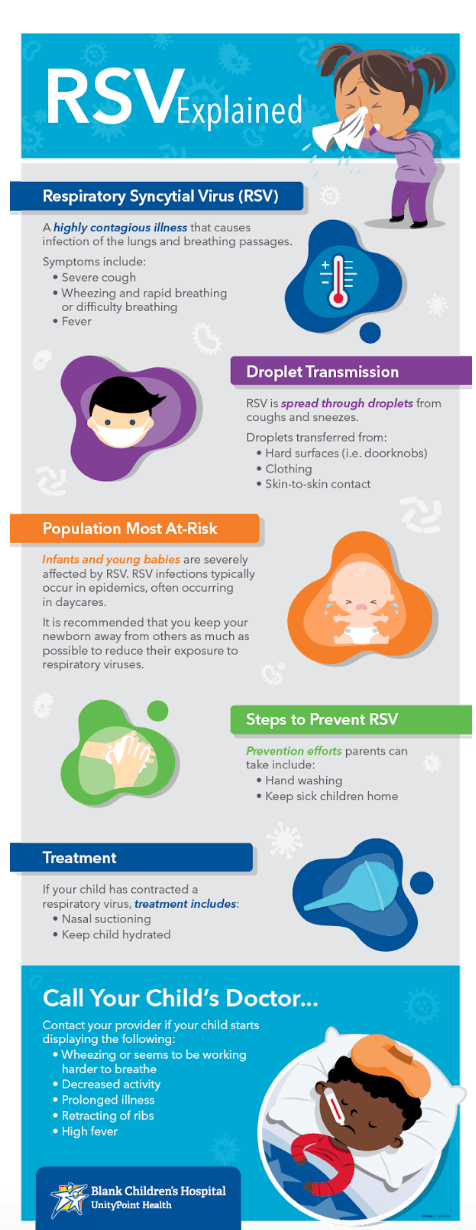
7. Respiratory Syncytial Virus (RSV)
- What is it?
- A viral infection in the smallest airways in the lungs caused by a virus called RSV.
- This is also commonly known as bronchiolitis.
- Symptoms:
- Wheezing is the most common symptom associated with RSV.
- Fast breathing, cough, fever, runny nose, eye drainage.
- Treatment:
- Warm mist to help with wheezing/cough
- Examples: steam from a hot shower or humidifier
- Increase fluid intake- give smaller more frequent meals/liquid if stuffy nose is making it hard for them to eat/drink.
- Some tricks for older babies and toddlers:
- Pedialyte popsicles
- Pedialyte Slushie (blend with ice)
- Clear juice (apple or pear) Slushie
- Breastmilk popsicles (try this popsicle mold)
- See our sick baby and toddler product recommendations here.
- Use nasal saline and suction to help relieve congestion.
- See our Reel for the suction trick!
- Some tricks for older babies and toddlers:
- Warm mist to help with wheezing/cough
- When to seek help:
- If you notice your baby/child is having trouble breathing you need to seek medical attention IMMEDIATELY (emergency room or call 911).
- Trouble breathing includes:
- Struggling to take a breath or shortness of breath
- Ribs are pulling in with each breath (retractions)
- Noisy breathing such as wheezing
- Fast breathing (usually greater than 40 breaths per minute)
- Lips or face turning blue
- Call your doctor: if fever lasts greater than 3 days, coughing worsens, you suspect that your child is dehydrated, trouble breathing but not severe, your child looks or acts very sick
8. Impetigo
- What is it?
- Skin infection caused by bacteria commonly found on skin.
- Examples include a scratch or insect bites that expose skin
- Highly contagious!
- Symptoms:
- Coin shaped sores on the skin covered by soft, yellow-brown scabs.
- Scabs may drain pus or yellow fluid that looks like honey.
- Usually start as small red bumps and then progress into larger size sores that drain and scab.
- Treatment:
- Soak off scabs by using warm water and mild soap.
- Apply a topical antibiotic ointment such as Bacitracin to the sores.
- Always talk to your provider before using.
- Apply a bandaid to sores to prevent any scratching and spreading.
- When to seek help:
- Call doctor now if you notice- pink or tea colored urine
- Fever and redness is spreading around the sores, your child acts or looks very sick.
- Notify your provider if your child has 3 or more impetigo sores (may need oral antibiotics), the sores do not improve after 1 week on antibiotic ointment, the sores get worse after 48 hours on antibiotic ointment, fever or sore throat occur.
9. Pink eye
- What is it?:
- A bacterial infection of the eye or eyes. Can also be viral.
- Symptoms:
- Pinkness in the white part of the eye, yellow or green discharge/pus in the eye
- Dried pus on the eyelids or eyelashes, eyelids are stuck/crusted together with pus after sleep
- Puffy eyelids
- Treatment:
- A prescription for antibiotic eye drops is usually recommended to clear the infection
- To remove pus:
- Use a soft cloth or cotton balls with warm water to gently remove pus or dried drainage
- Be sure to wipe from the inside corner of the eye to the outside and dispose of the cloth/cotton ball to avoid spreading infection.
- Be sure to remove pus before giving eyedrops- they won’t be effective if pus is in the way of the antibiotic getting to the eye!
- Use a soft cloth or cotton balls with warm water to gently remove pus or dried drainage
- When to seek help:
- Eyelid is very red or swollen, severe eye pain, fever of 104 degrees F, baby is less than 12 weeks old with a fever, your child looks or acts very sick.
- Call your provider if pus is still present after 3 days of using antibiotic eyedrops.
10. The Flu – Norovirus vs. Influenza
Norovirus
- What is it?
- A gastrointestinal infection from a virus (rotavirus is the most common)
- Symptoms:
- Vomiting
- Watery-loose stools
- Nausea, low appetite
- Drowsiness but arousable
- Treatment:
- Bottle fed babies:
- Spoon or syringe feed small amounts of an oral rehydration solution (unflavored pedialyte or organic pedialyte ).
- Contact your provider before starting.
- Give 1-2 teaspoons(5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- After 8 hours without throwing up, go back to regular formula/breastmilk.
- Contact your provider before starting.
- Spoon or syringe feed small amounts of an oral rehydration solution (unflavored pedialyte or organic pedialyte ).
- Direct breastfed babies:
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes.
- Contact your provider before starting.
- After 4 hours without throwing up, return to regular nursing. If continues to vomit, switch to pumped breastmilk.
- Spoon or syringe feed small amounts of pumped milk.
- Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes.
- As your baby keeps down the smaller amounts, slowly give more. An oral rehydration solution (unflavored pedialyte or organic pedialyte) can be used if vomiting becomes worse.
- Avoid all solid foods and baby foods in kids who are vomiting. After 8 hours without throwing up, gradually add them back. Start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Bottle fed babies:
- When to seek help:
- Call your doctor if: you suspect dehydration- no urine in more than 8 hours, dark urine, no tears when they cry, and dry mouth. Stomach pain when not vomiting, severe vomiting for more than 8 hours.
- Go to ER if: it is hard to wake your child up, they act or talk confused, have severe abdominal pain, blood or bile (bright green color) in their vomit.
- Call 911 if: you are unable to wake up your child, they are took tired/weak to stand or move.
Influenza
- What is it?:
- A viral respiratory infection caused by the influenza virus that changes yearly
- Symptoms:
- Fever with a runny nose, sore throat, and a bad cough. Can also have muscle pain/aches, headache and chills.
- Treatment:
- Blow or suction the nose frequently: use nasal saline and suction for younger children/babies and teach older children to blow their noses frequently to relieve congestion.
- see our Reel for the suction trick!
- Increase fluid intake.
- Some tricks for older babies and toddlers:
- Pedialyte popsicles
- Pedialyte Slushie (blend with ice)
- Clear juice (apple or pear) Slushie
- Breastmilk popsicles (try this popsicle mold)
- See our sick baby and toddler product recommendations here
- Treat fever and body aches with acetaminophen or ibuprofen
- Please contact your provider for accurate doses. Please note that children under 6 months of age cannot receive Motrin (ibuprofen).
- Antiviral drugs, such as Tamiflu, are sometimes used to treat influenza- it must be started within 48 hours of when symptoms started or else the drug is not effective (get prescription from your provider).
- The AAP recommends that only children with severe influenza symptoms should be treated with antiviral drugs.
- Blow or suction the nose frequently: use nasal saline and suction for younger children/babies and teach older children to blow their noses frequently to relieve congestion.
- When to seek help:
- Call your doctor if: fever lasts more than 3 days, you suspect dehydration, you notice noisy breathing (wheezing/stridor), you notice faster breathing (greater than 40 breaths per minute), trouble breathing but not severe.
- Go to the ER if: breathing is becoming more difficult, you notice ribs pulling in (retractions), your child seems “out of it” or not alert when awake.
- Call 911 if: you child is having severe trouble breathing, lips or face are blue when not coughing, you cannot wake your child up
Additional illness we wanted to include: Febrile Seizures
- What is it?
- A seizure that usually occurs within the first few hours after a fever has started.
- Typically caused by a spike in body temperature resulting from an infection.
- Symptoms:
- Fever
- Stiffening of the body, twitching, eye rolling, repetitive movements of the arms or legs
- Unresponsive for a short period of time, breathing may be disturbed, skin may appear discolored.
- Typically last less than 1 minute.
- CALL 911.
- Treatment: If you notice your child having a seizure:
- Place them on the floor and away from any hard or sharp objects.
- Turn their head to the side for any saliva or vomit to easy drain from their mouth
- Do not put anything in their mouth!
- When to seek help:
- Call 911 if seizure does not stop after 5 minutes or if you are concerned about your child’s breathing
- Call your pediatrician to notify them of the seizure and for further instructions/care
**Febrile seizures are scary but they are NOT harmful to your child. They do not cause brain damage, nervous system problems, paralysis, intellectual disability, or death.
How to maximize pain and fever control in babies and toddlers:
**Motrin can only be used for infants greater than 6 months, always check with pediatrician before starting any new medications.
**Be sure to read dosage/instructions on the back of the medication box before administering.
Tylenol (acetaminophen) should only be given a minimum of every 4 hours
Motrin (ibuprofen) should only be given a minimum of every 6 hours
These mediations can be given in combination with one another but it is important to keep in mind the times at which they are administered so you aren’t giving them earlier than what is considered safe.
**Fever is considered anything greater than 100.4 degrees Fahrenheit
Example:
- 12pm: baby wakes up from nap with a fever
- Give Motrin (cannot administer again until 6pm)
- 1pm: check temperature again- baby still has a fever
- Give Tylenol (cannot administer again until 5pm)
- 2pm: check temperature
- Cannot give either mediation if still febrile)
- 3pm: check temperature
- Cannot give either medication if still febrile)
- 4pm: check temperature
- Cannot give either mediation if still febrile)
- 5pm: check temperature- baby still has a fever
- Give Tylenol (safe to give again because it has been 4 hours since the last dose)
- 6pm: check temperature- baby still has a fever
- Administer Motrin (safe to give again because it has been 6 hours since the last dose)
**Continue to alternate these medications if the baby is still running a fever/feeling unwell.
**Notify pediatrician immediately of a fever in infants less than 3 months of age or a fever lasting greater than 48 hours in infants/children greater than 3 months old.
Have more questions? Schedule a text or video chat consult with Kate, Lauren or Natalie (NICU RNs) and they can help answer any questions that you have!
BOOK CONSULT NOW
Other helpful blog posts:
- Medicine Kit Essentials
- First Aid Kit Essentials
- How to care for your baby’s umbilical cord
- Sick baby and toddler essentials
- Everything you need to know about thrush
- Newborn acne – when should I worry?
- Kate’s effective diaper rash remedy
Amazon store:
**This post is educational and not meant to take the place of your provider. Bumblebaby makes a small commission on some of the items listed above